tear break up time test reimbursement|cost of tear testing : factory Separate reimbursement for tear production measurement (Schirmer test), tear break-up time (TBUT), dye disappearance testing (sodium fluorescein), Jones dye testing or .
Max Q Lynn Barebacks Black Gay Booty in Raw Threesome .
{plog:ftitle_list}
(MFA will most likely NOT become available as a download.) .
A High Lf: > 1.0 mg/ml and a Low Lf: < 0.8 mg/ml (AXIM, 2021). Additional Tests. Other tests noted by the American Academy of Optometry (AAOPT) are the tear break-up time test, the .
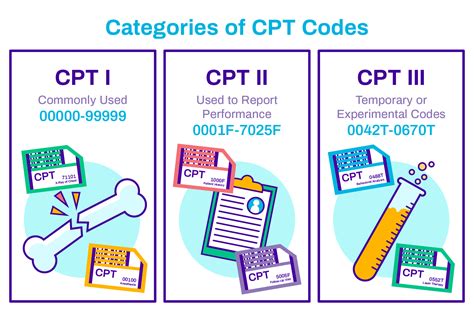
Jones II test: The test itself is not billed, but it may involve probing and irrigation of the canalicula; if so, CPT code 68840 is proper. Tear osmolarity (TearLab, TearLab): CPT laboratory test 83861 – distributed as “TearLab”* • A diagnosis of aqueous tear deficiency confirmed by one or more of the following diagnostic tests: tear break-up time (TBUT), Schirmer test, ocular surface dye staining . What is Tear Break-Up Time Test? The Tear Break-Up Time (BUT) Test is a clinical assessment used to evaluate the stability of the tear film on the ocular surface, .
Tear prism evaluation. Biomicroscopy. Once youve diagnosed a patient with dry eye syndrome and formalized a treatment plan, youll typically require several subsequent . Separate reimbursement for tear production measurement (Schirmer test), tear break-up time (TBUT), dye disappearance testing (sodium fluorescein), Jones dye testing or . The current national reimbursement amount for this lab test is .52 per eye. • 0330T. “Tear film imaging, unilateral or bilateral, with interpretation and report.” This code for .Physical examination usually reveals reduced tear volume or quality, decreased tear break-up time and corneal surface changes. Because DES is a medical condition, you should submit .
To test TBUT, a drop of fluorescein dye is placed in the eye, the patient blinks a few times to spread the dye across the eye’s surface, and the doctor counts the seconds before the tear .Separate reimbursement for tear production measurement (Schirmer test), tear break-up time (TBUT), dye disappearance testing (sodium fluorescein), Jones dye testing or saccharine testing is not available. These are considered part of a general opthalmological examination or E&M service. 3. Reimbursement for CPT 68801 and 68810 is limited to . The lack of stability can be measured by the tear break-up time (TBUT) as the interval of time that elapses between the end of a complete blink and the appearance of the first break in the tear .
La Trobe Orthoptics students present an instructional video on the clinical test of measuring tear break up time (TBUT). ORT5CLA Clinical skills group video . Le temps de rupture du film lacrymal ou BUT est un test clinique fiable de réalisation simple qui peut être utilisé pour confirmer le diagnostic de sécheresse oculaire. Summary. Introduction. Dry eye disease (DED) can be evaluated clinically by the tear film break up time (BUT). There is a discrepancy between symptoms in relationship with . In the realm of ophthalmology, precise measurement of tear film break-up time (TBUT) plays a crucial role in diagnosing dry eye disease (DED). This study aims to introduce an automated approach . An incidental test can be done by the technician or the provider and no code applies. Here’s a partial list of incidental dry eye tests: Schirmer tear testing (type I or II) Tear break-up time (TBUT) Phenol Red thread; Rose bengal testing; Dye disappearance test; Jones I test; Tear meniscus height; Examination at the slit lamp (w/ or w/o dye .
Physical examination usually reveals reduced tear volume or quality, decreased tear break-up time and corneal surface changes. Because DES is a medical condition, you should submit examination and diagnostic testing reimbursement claims to Medicare or other medical insurance, not to vision insurance, which covers eyeglass and contact lens .
requirements of a valid co-morbidity or medical reimbursement. Diagnosis codes that describe signs and symptoms (e.g. headache, pain in or around the eye, visual . • Tear break up time • Schirmer and ocular surface testing • Corneal sensation . • Tear film adequacy • Schirmer's test • Slit lamp (biomicroscopy) • Fundus examination Non-Invasive Tear Break-up Time Test. The second version of the TBUT test is the noninvasive tear break-up time (NI-BUT) test, which has been developed based on advancements in computer and software systems and is performed with devices integrated into corneal topographic instruments or specialized only for this test [2], [10], [12] – [16]. • A diagnosis of aqueous tear deficiency confirmed by one or more of the following diagnostic tests: tear break-up time (TBUT), Schirmer test, ocular surface dye staining pattern (Rose Bengal, fluorescein, or lissamine green); and .
tear lab clia waiver
Tear film break-up time Test:• The BUT is the interval between the last blink and the appearance of the first randomly distributed dry spot. • A . Tear production measurement (Schirmer test), and tear break-up time (TBUT) can indicate insufficiency or instability of tears, which can cause or contribute to epiphora. Dye disappearance testing (sodium fluorescein), Jones dye testing or saccharine testing can be used to exclude significant obstruction and/or help identify the site and degree .
Optometrist Susan Bowers explains how to measure a patients tear break up time
The aim was to determine feasibility and reliability of noninvasive tear break-up time (NIBUT) assessment using handheld lipid layer examination instrument, and to compare it with standard tear break-up time (TBUT) test. Fifty patients were enrolled, 31 with and 19 without dry eye symptoms. Schein q . Be sure to maximize amount of dye in tear film to avoid false negatives c. Observe using white light d. Measure location and intensity of staining e. Stains areas of devitalized epithelium (missing mucin layer) C. Tear .questionnaires, tear film break-up time (TFBUT), Schirmer test, ocular surface staining, and meibomian gland functionality. However, many of these tests lack consistency and reliability in diagnosis. New tools have been developed which allow for the quantification of tear film characteristics including measurement of tear osmolarity
Increased use and reimbursement: Evidence supporting the benefit of the tear osmolarity test is the increased use by eye care specialists. The difference in reimbursement and cost of supplies does not cover the technician's or the physician's time required to perform the test.diagnostic tests may include tear break-up time (BUT), Schirmer’s tear test, and staining with rose bengal, fluorescein or lissamine green. Some doctors employ a lactoferrin assay to detect protein abnormalities in tears. Any one or more of these tests can be used to help support the diagnosis of dry eye syndrome. This study aims to investigate the reliability and efficacy of maximum fluorescein tear break-up time (FTBUTmax) in diagnosing dry eye disease (DED). 147 participants were enrolled in this study.
First and foremost, punctal plugs should be considered in all cases of aqueous-deficient DED, i.e. those individuals who show diminished tear volume (as measured by Schirmer strips, phenol red thread test or direct measurement of the tear meniscus), reduced tear stability (rapid tear break-up time) and a symptom profile consistent with dry eye.If a person keeps their eyes open long enough, without blinking, their tear film will start breaking up. This makes the eye feel uncomfortable and forces you to blink to maintain comfort. In patients with dry eyes, the tear film is unstable and tends to break up faster. This may entail a brief overview of the nature of dry eye, and can include pointers on the influence blinking has on the tear film and ocular surface protection, especially during visual tasking, or how to estimate tear film break-up at home using a simple test called the symptomatic break-up time (SBUT). This test involves a patient holding . Tear film quality has most commonly been monitored using tear break-up time with application of sodium fluorescein, which in itself is known reduce the stability of the tear film. 6 Non-invasive tear break up time (NIBUT) can be obtained from placido disc images reflected by the cornea from the tear film, and can be done with many of the .
standard tear break-up time (TBUT) test. Fifty patients were enrolled, 31 with and 19 without dry eye symptoms. Schein questionnaire was used to assess dry eye symptoms. During examination, three
cpt code for tear testing
tear test of fabric
Testing such as tear film break up time (TBUT), Schirmer test, vital dye staining (lissamine green, fluorescein, rose bengal) and biomicroscopy examination cannot be charged separately because they are included in any medical management code that can be used. . At this time, there is not a specific code that can be used that properly .
Tear Break-Up Time (TBUT) is a crucial diagnostic test used in optometry to assess the stability of the tear film, an important factor in eye health and comfort. This test measures the interval between a complete blink and the appearance of the first dry spot on the corneal surface after the instillation of a fluorescein dye. Tear break-up time (TBUT) remains one of the most commonly employed tests to assess tear film stability and for dry eye diagnosis [1,2]. First introduced by Norn in 1969, TBUT was defined as the time “interval between the last complete blink and the presentation of the first appearance of a dry spot or disruption in the tear film” [2,3]. While many variations exist, the .

tear test plastic film
cpt code for tear film
Resultado da 1 de jun. de 2023 · Texto: Português | Multi. Lançamento: 2020. Crack: Incluso. Plataforma: PC. Tipo de link: Magnet Link. Descrição: Black Mesa Torrent é um remake do clássico jogo de tiro em primeira pessoa Half-Life, lançado originalmente em 1998. O jogo se passa em uma instalação de .
tear break up time test reimbursement|cost of tear testing